Objectives
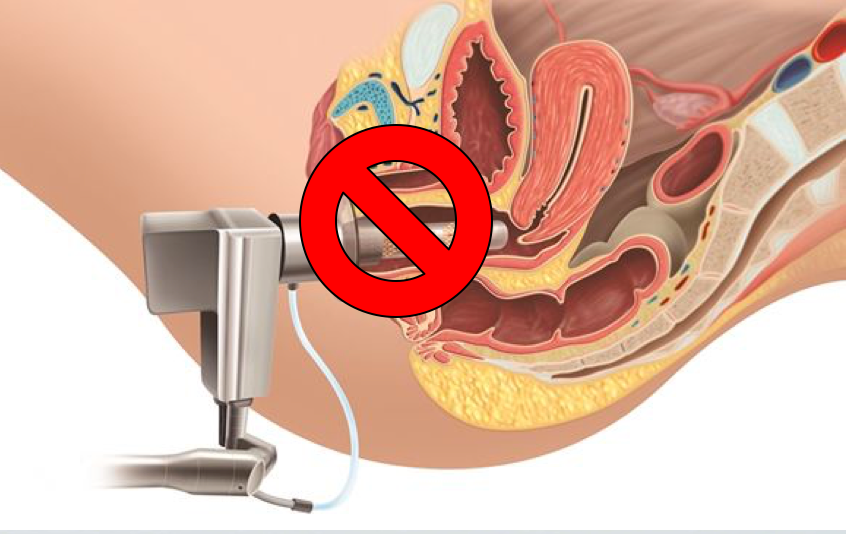
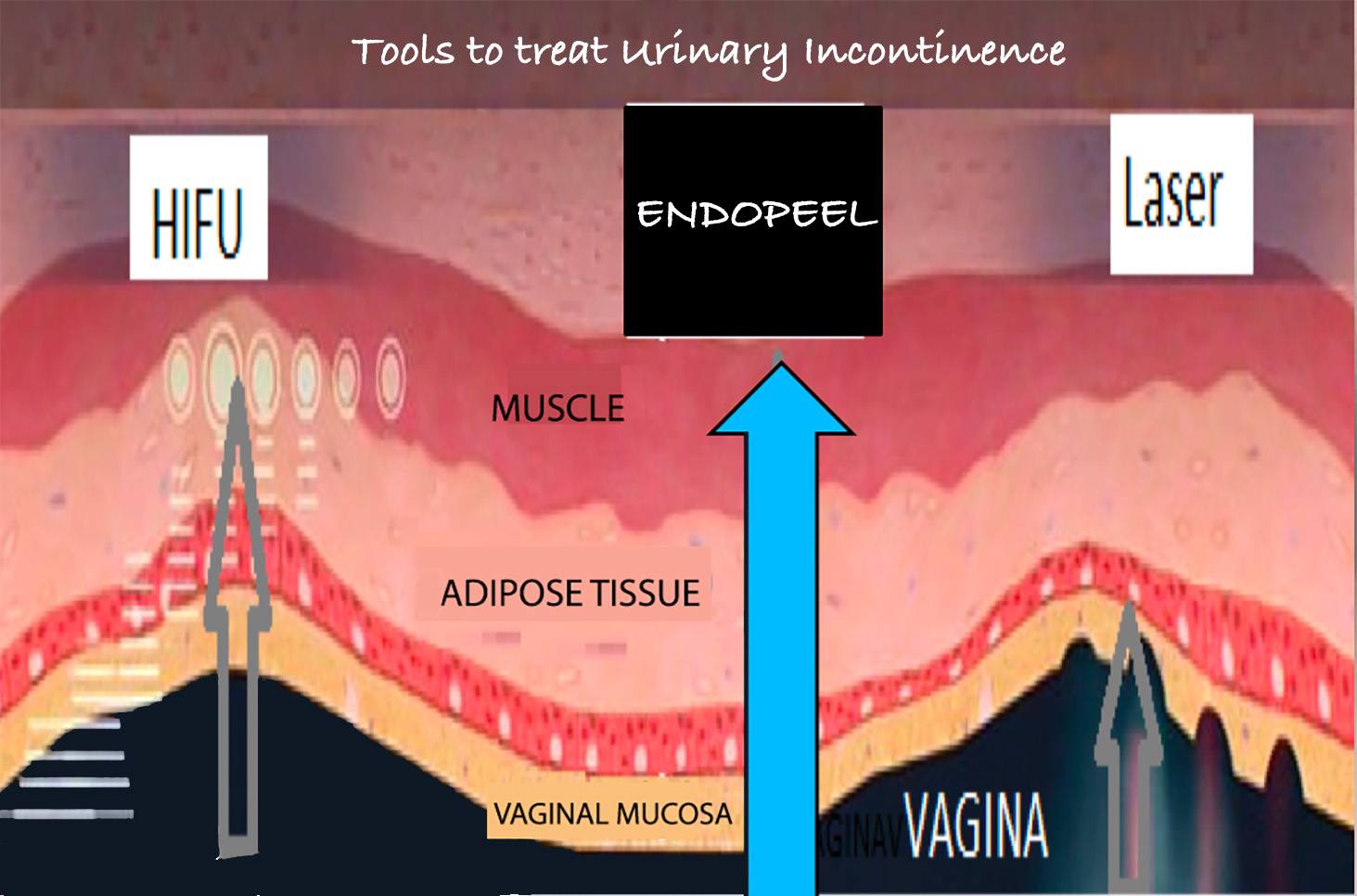
BEFORE 2018 , all treatments were using surgery, laser. HIFU.
Their goal was to correct THE HYPER URETRAL MOTILITY.
NOWADAYS, we propose less invasive treatments using:
ENDOPEEL



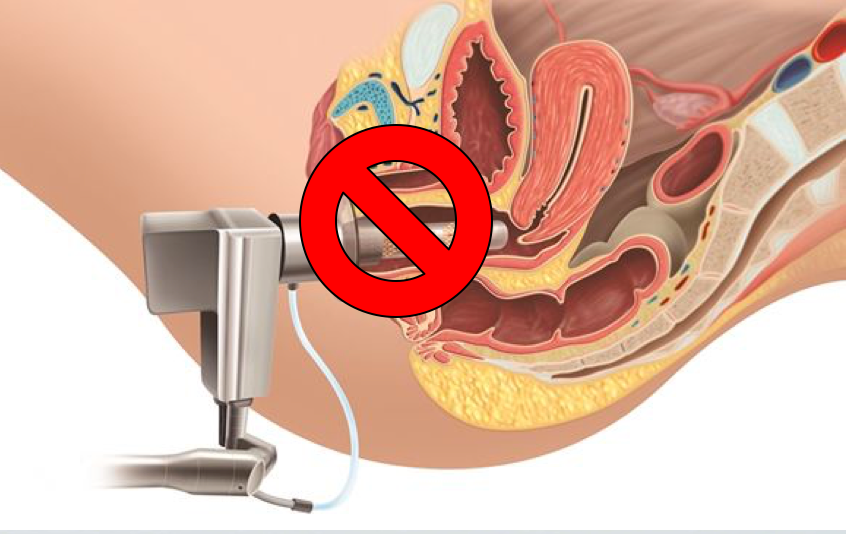

BEFORE 2018 , all treatments were using surgery, laser. HIFU.
Their goal was to correct THE HYPER URETRAL MOTILITY.
NOWADAYS, we propose less invasive treatments using:
ENDOPEEL





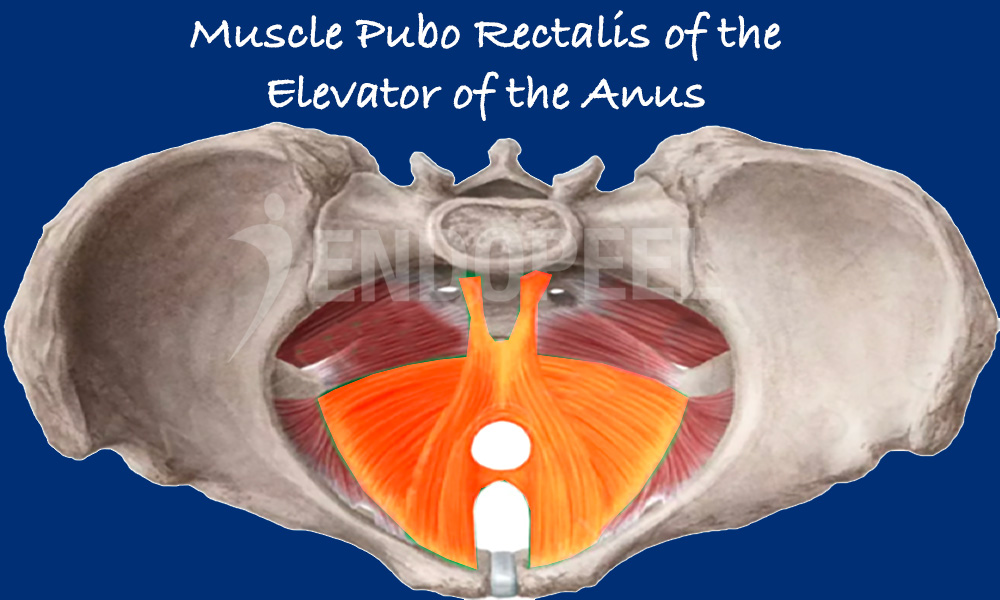
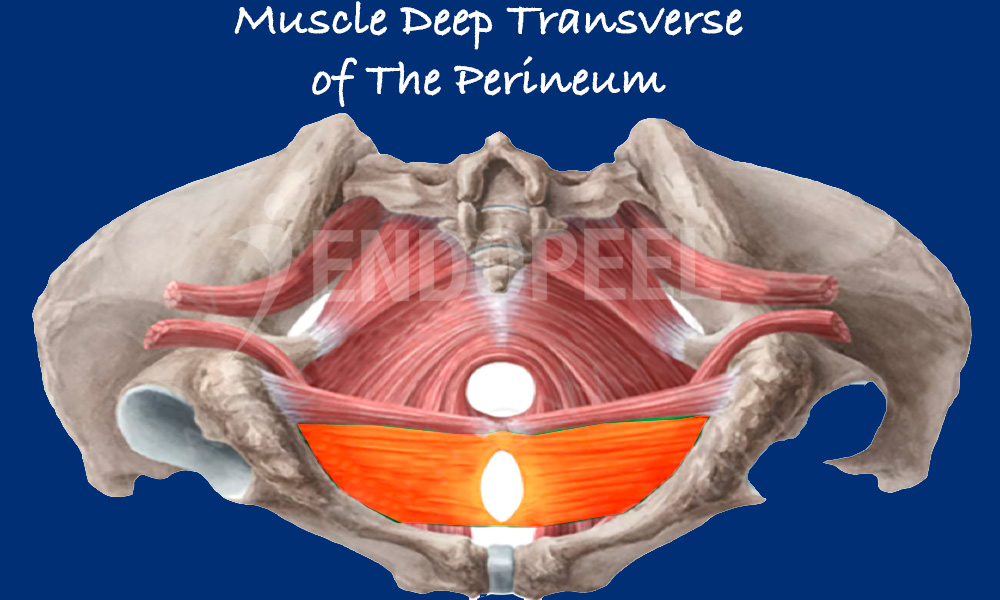
The goal is to get a 3D isovolumetric myoplasty, myopexy and myotension of the puborectalis of the elevator of the anus and deep transverse of the perineum.
In case you add threads, use a resorbable mesh,
in the fatty layer of the urethro-vaginal space.
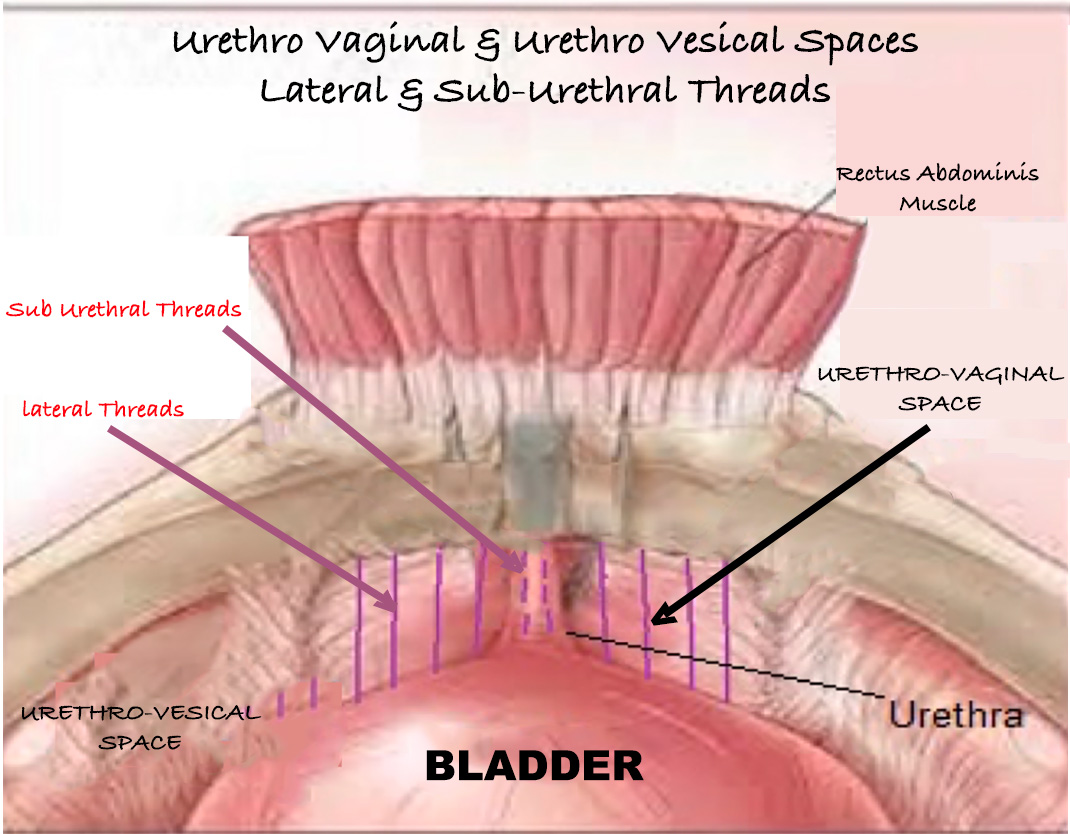
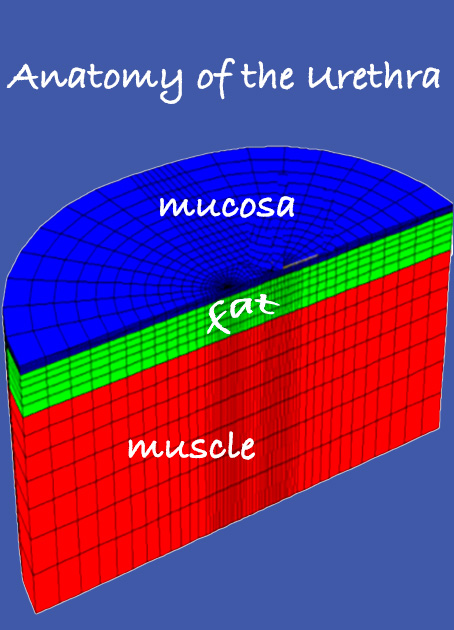
with its 3 layers
fenestrated ( window) vaginal speculum with urethral protection made by Dr.Alain Tenenbaum & Prof.Dr.Mohan Thomas






The continuous line marks the horizontal with respect to the pubic
the discontinuous line marks the mobility of the urethra, which is obtained from the difference between A and B (rest and effort)
Study realized between November 2016 till August 2017
on
MATERIAL & METHODS
N=40 female patients
Age Range : 40-62 years old
With 31 patients Grade I
And 9 patients Grade II
ALL TREATED WITH ENDOPEEL-THREADS as described above
RESULTS FOR GRADE I
RESULTS FOR GRADE II
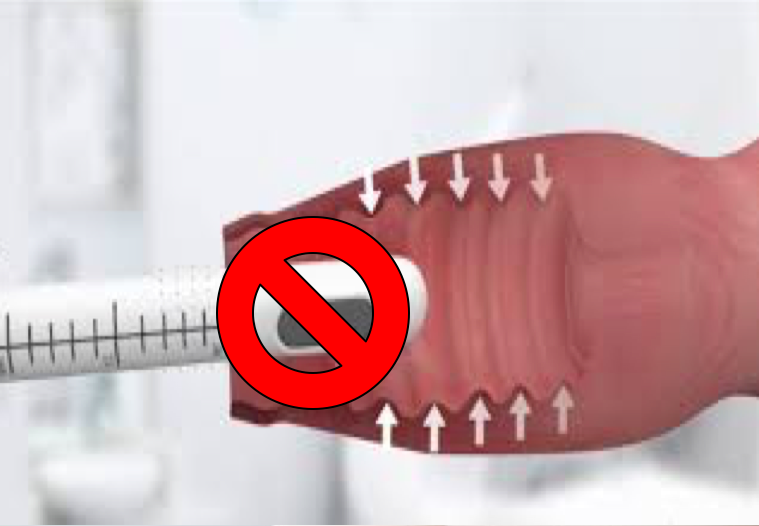
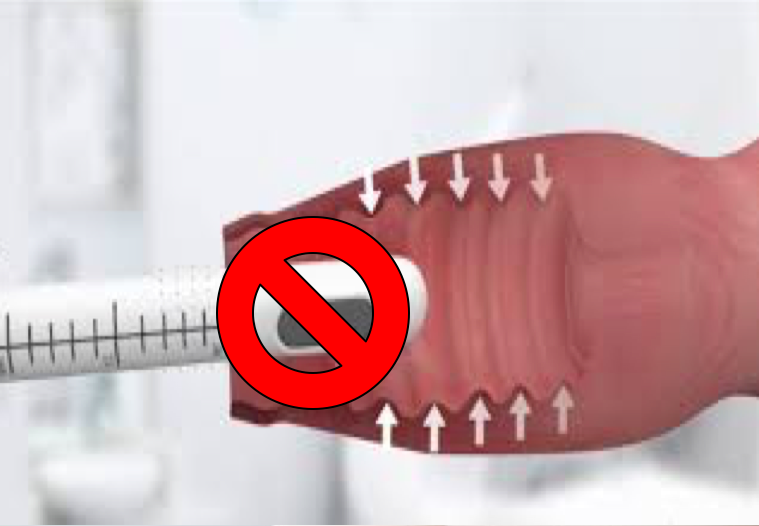
PRP and Urinary Incontinence: A Critical Perspective
Despite widespread marketing claims, Platelet-Rich Plasma (PRP) has no scientifically proven efficacy in the treatment of urinary incontinence. While PRP may enhance superficial tissue trophicity in cases of vulvovaginal atrophy, it does not act on the muscular tone or closure mechanism of the urethral sphincter.
PRP is often promoted by individuals with no formal training in pelvic floor medicine, and in some cases by those with a history of scientific data manipulation. These unproven claims mislead physicians and expose patients to treatments that lack both safety and efficacy.
In contrast, Endopeel has shown consistent and immediate results by increasing the functional tone of both smooth and striated muscles, including the puborectalis, the deep transverse perineal muscle, and the urethral sphincter. This increase in muscular tension leads to effective tightening and improved continence.
Several independent urologists have clinically confirmed the positive impact of Endopeel on urinary control, particularly in cases of stress or mixed incontinence. Unlike PRP, Endopeel works within hours and does not rely on speculative regenerative processes.
We encourage clinicians to remain vigilant and to critically evaluate therapeutic claims, especially when they are linked to commercial interests or unsupported by rigorous, peer-reviewed science.
